Custom blending of radiopaque fillers can increase the opacity of catheters and other devices, making them clearly visible under fluoroscopy and x-rays without sacrificing much of the physical properties of the polymers. Radiopaque formulations incorporated into medical device components enable surgeons to view positioning and placement live during the procedure. Proper visualization is key to many procedures that require the use of catheters, guidewires, and stents to ensure proper placement and deployment, specifically in the cardiovascular space.
Polymers used to produce catheters and other devices that are inserted into the body for diagnostic or interventional procedures are commonly filled with substances opaque to x-rays, thereby rendering the devices visible under fluoroscopy or x-ray imaging. These fillers, or radiopacifiers – typically dense metal powders – affect the energy attenuation of photons in an x-ray beam as it passes through matter, reducing the intensity of the photons by absorbing or deflecting them. Because these materials exhibit a higher attenuation coefficient than soft tissue or bone, they appear lighter/brighter on a fluoroscope or x-ray film. This visibility provides the contrast needed to accurately position the device in the affected area. Image contrast and sharpness can be varied by the type and amount of radiopacifier used and can be tailored to the specific application of the device.
For example, a device designed for use near the surface of the skin requires less radiopaque filler to achieve the required level of attenuation compared with one used inside the coronary vasculature. Device design is also a factor. A higher loading of radiopaque material, for instance, is needed for thin-wall catheter tubing than for products with thicker walls. Generally, compounds should contain only the amount of additives absolutely required for the application, since overloading can result in the loss of the mechanical properties of the polymer. Additionally, blending several radiopaque materials can produce better results than using only one type in a formulation.
Among the most widely used radiopacifiers for medical devices are barium sulfate, bismuth compounds, and tungsten metals that are excellent absorbers of x-rays. Selection of the correct fillers in the proper amount requires a thorough understanding of attenuation and how it is affected by various radiopaque compounds. This article discusses those radiopaque fillers commonly used with medical-grade thermoplastic polymers and the factors involved in their selection.

Understanding X-rays
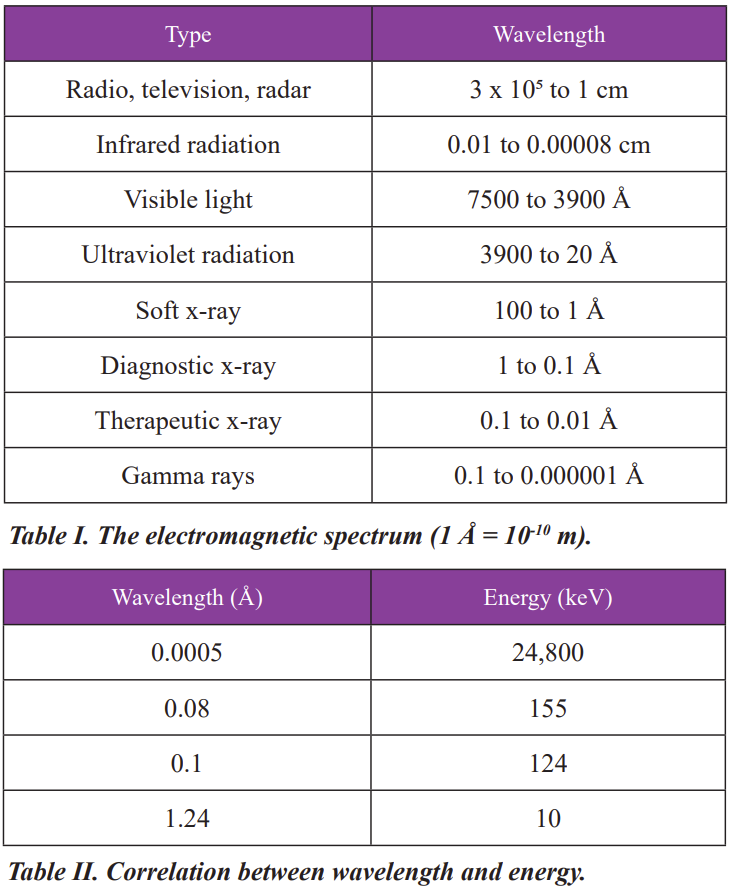
X-rays are a form of radiation and are part of the electromagnetic spectrum consisting of energy waves of widely differing frequency and length. Produced by the oscillation or acceleration of an electric charge within a magnetic field, these waves range from those with very high frequencies and short wavelengths to those with very low frequencies and long wavelengths (Table I).
Diagnostic x-rays fall near the shorter-wavelength end of the spectrum, measuring between 1 Å – about 4 billionths of an inch long – and 0.1 Å. X-rays are produced from the conversion of energy that results when fast-moving electrons from the filament of an x-ray tube interact with a tungsten anode or target. The kinetic energy of the electrons increases as voltage, expressed as peak kilovoltage (kVp), is increased. The intensity of an x-ray beam is determined by the number of photons in the beam and the energy of the photons, which is expressed as kiloelectronvolts (keV).
Shorter wavelength x-rays exhibit greater energy and penetrating power than longer wavelength x-rays (Table II). For example, 0.1 Å is equivalent to about 124 keV of energy, while 1.24 Å equals only 10 keV. A voltage of 100 kVp – the standard rating of older-model x-ray machines – will not have all photons at 100 keV. Typically, 100 kVp produces < 1% of photons at a 0.1 Å wavelength, whereas the other 99% are longer and have less energy. Photons with ≥15 keV can ionize atoms causing the loss of an electron to produce ionizing radiation. Gamma rays, x-rays, and some UV rays are considered ionizing radiation.
Energy attenuation relates both to the quantity and the quality of the photons in a beam. Increasing the energy increases the number of photons transmitted and generally decreases the degree of attenuation. The precise nature of the radiation affects attenuation, as does the density, atomic number, and electrons per gram of the absorbing or radiopaque material. An increase in any of these factors decreases the number of transmitted photons and thus increases attenuation.
In an x-ray beam, both the transmitted and attenuated photons are important in producing an accurate image. Different types of tissues attenuate energy differently, which provides contrast in the x-ray image. A dense element such as barium, with an atomic number of 56, has a higher attenuation coefficient and absorbs x-rays better than matter that is less dense. The higher the attenuation coefficient, the lower the number of transmitted photons. Density, which is directly proportional to attenuation, determines the number of electrons that are present in a given thickness of material and, thus, the photon-stopping power. Denser materials appear as lighter or brighter images on an x-ray film or a fluoroscope, which displays a moving image when a beam of penetrating radiation is transmitted through the body onto a viewing screen.
Differences between attenuation of bone and soft tissue under low-energy radiation are produced by differences in the number of photoelectric reactions, which involve the formation and liberation of electrons during electromagnetic radiation. The calcium in bone has a higher atomic number than that of the surrounding tissue, causing more reactions and increased attenuation. At higher energy levels, however, variations in attenuation depend more on interactions known as Compton scatterings, which are changes in wavelength that occur when the waves are scattered.
As mentioned, x-ray transmission generally increases, and attenuation decreases when the radiation energy of a beam is increased. But this does not hold true with high-atomic-energy absorbers such as, for example, iodine (atomic number 53). Transmission may decrease with increased beam energy because of the likelihood of a photoelectric reaction occurring as the energy approaches the binding energy of an inner-shell electron. A photon needs a minimal amount of energy – more than the binding energy of the electron – to eject an electron. High-energy photons are thus less likely to be transmitted than low-energy photons.
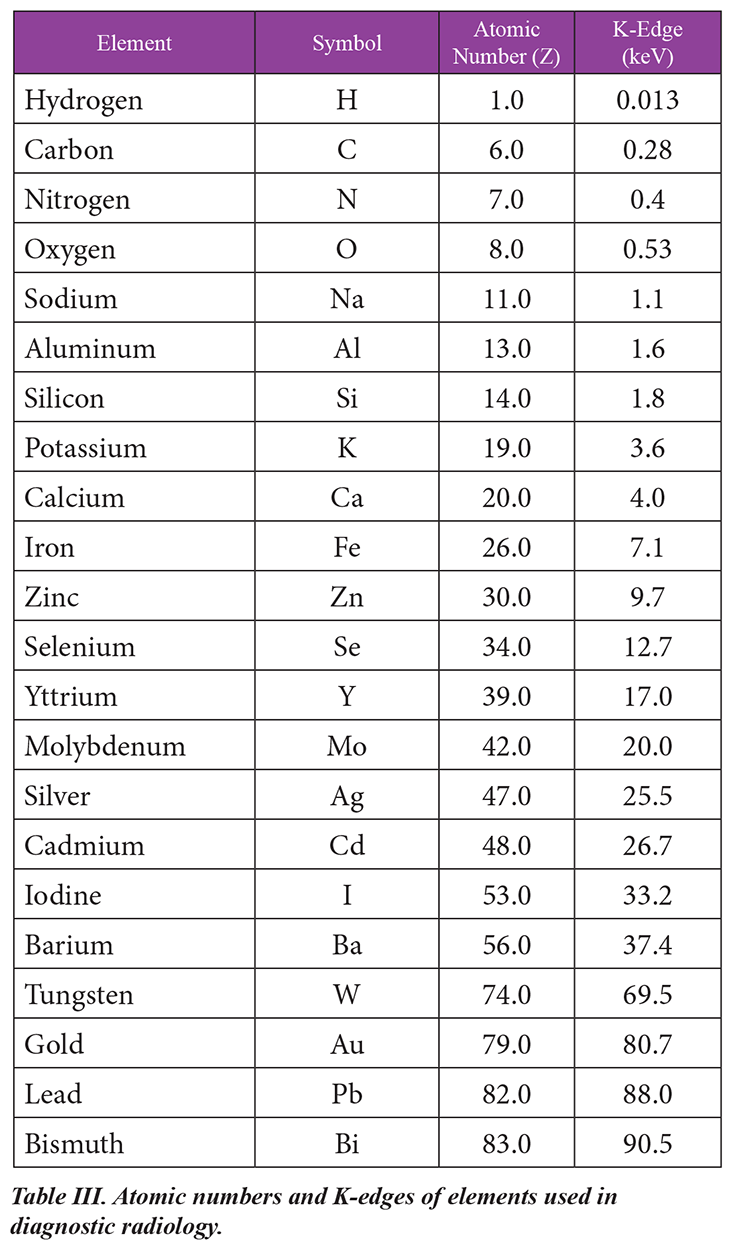
For some elements, an important property for diagnostic radiology is the K-shell binding energy, known as the K-edge (Table III). For example, an x-ray of 33 keV will not eject an electron from the K-shell of iodine, which has a K-edge of 33.2 keV. A photoelectric reaction has a greater chance of occurring when the photon energy and electron binding energy are nearly the same: that is, a 3O-keV photon is more likely to react with the K-shell electron of iodine than is a 100-keV photon. Because electrons that are tightly bound in their orbits are most likely to be involved in photoelectric reactions, the K-edge of the absorber should be near the energy of the x-ray beam to ensure maximum x-ray absorption.
Polychromatic radiation, which contains photons of varying energies, is more complex in terms of attenuation than monochromatic radiation. Both the quantity and quality of photons in a polychromatic beam change as they pass through an absorber. The peak kilovoltage of a polychromatic beam determines the mean energy, which falls between ⅓ and ½ of the peak, so that a 100-kVp beam has a mean energy of about 40 kV. In the case of a 100-kVp x-ray machine, barium, with a K-edge of 37.4 keV, is an excellent absorber. When the mean energy increases significantly, tungsten, with a K-edge of 69.5, becomes a better choice as a radiopaque material.
Common Radiopacifiers
Barium Sulfate
Barium sulfate (BaSO4) was the first radiopaque material to be widely compounded in medical formulations and is the most common filler used with medical grade polymers. (Patients are often asked to swallow a solution of barium sulfate before an examination of their digestive tract.) Its white color can be changed with the addition of colorants.
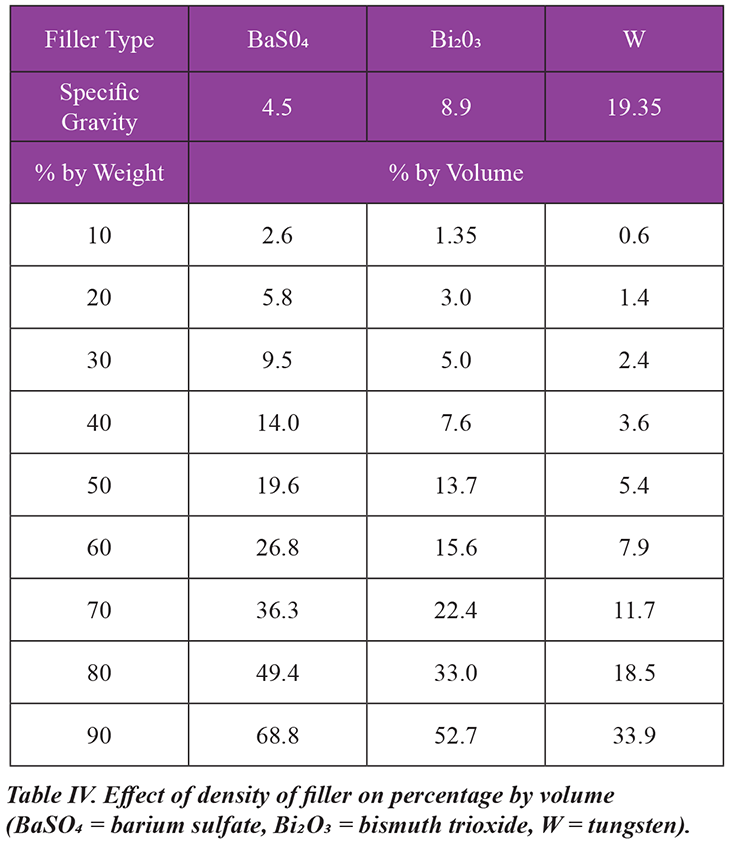
With a specific gravity of 4.5, barium sulfate is generally used at loadings of 20% to 40% by weight. While a 20% barium sulfate compound is typical for general-purpose medical device applications, some practitioners prefer a higher degree of radiopacity than can be provided by that loading. With striped tubing, for example, a 40% compound is standard.
A loading of 20% barium sulfate by weight is equivalent to about 5.8% by volume; 40% by weight equals 14% by volume (Table IV). As the barium content moves beyond about 20% by volume, compounds begin to show losses of the base polymer’s tensile strength and other mechanical properties. It is therefore best to formulate radiopacifiers at the minimum level for each application; excessive use of these fillers is not recommended.
Bismuth
Considerably more expensive than barium, bismuth compounds are also twice as dense. Bismuth trioxide (Bi2O3), which is yellow in color, has a specific gravity of 8.9; bismuth subcarbonate (Bi2O2(CO3)) has a specific gravity of 8.0; and bismuth oxychloride (BiOCI) has a specific gravity of 7.7. Because of the density, a 40% bismuth compound contains only about half the volume ratio as a 40% barium sulfate compound. Since bismuth produces a brighter, sharper, higher-contrast image on an x-ray film or fluoroscope than does barium, it is commonly used whenever a high level of radiopacity is required.
Compared with barium, higher loadings are also possible: even a 60% bismuth compound can maintain the same base polymer mechanical properties as a 40% barium sulfate compound. A 20% bismuth loading by weight equals 3% by volume; a 40% loading by weight equals 7.6% by volume. Bismuth is sensitive to compounding and must be treated gently, with low-shear mixing recommended for optimum results. Because of their high levels of radiopacity, bismuth fillers have grown in popularity.
Tungsten
A fine metal powder with a specific gravity of 19.35, tungsten (W) is more than twice as dense as bismuth and can provide a high attenuation coefficient. A loading of 60% tungsten has approximately the same volume ratio as a 40% bismuth compound. Devices can be made highly radiopaque with relatively low loadings of tungsten, enabling good mechanical properties to be maintained. Because of its density, tungsten is typically selected as a filler for very thin-walled devices.
A 50% tungsten loading by weight equals only 5.4% by volume, and an 80% loading by weight represents 18.5% by volume. Tungsten is black in color, which cannot be changed with colorants. It is abrasive and can cause accelerated wear in extruders and other processing equipment. Devices filled with high loadings of tungsten will exhibit surface roughness. Because the material invites oxidation in the presence of oxygen and heat and is highly flammable, care should be taken while drying it. With elastomers, barium sulfate mixes better than tungsten or bismuth compounds.
Compounding Considerations
Newer x-ray machines generally operate at higher energy levels than older ones, typically at 80 to 125 kVp compared with 60 to 80 kVp for older machines. Higher energy radiation increases the transmission of photons and can require higher levels of radiopacity to provide the desired attenuation.
Therefore, devices produced with barium sulfate compounds might not appear as bright on newer machines, for which bismuth compounds would be a better choice of radiopaque filler. Blending these materials, however, can often be the best solution, especially for multipurpose formulations used over a broad range of energy levels. A blend of barium, easily attenuated at low energy levels, and bismuth, attenuated at higher levels, often works well.
Conclusion
Medical devices used in diagnostic radiology must be easily seen on x-ray film and fluoroscopes for medical practitioners to precisely position them inside the body during critical procedures. The type and amount of radiopaque filler compounded with thermoplastic materials in the manufacture of these devices determines how they appear. The filler affects the degree of contrast and the sharpness of the image to the extent that it influences the attenuation of x-rays passing through the body and the device.
Successful material selection starts with an understanding of x-ray energy and attenuation. The effectiveness of the filler is related to the energy level of the x-ray equipment, the wall thickness of the device, the location inside the body where the device will be used, and the required mechanical properties of the polymer. The best compound for a specific application is often a blend of radiopaque fillers – such as a barium sulfate and bismuth compound – that provides the desired level of attenuation without the excessive loading that can degrade the mechanical properties of the polymer.
For a downloadable PDF of this white paper, click here.